Understanding the Breakdown and Consequences of Incomplete Fat Metabolism
Ketosis is a metabolic state in which the body uses fat as a primary energy source because of limited glucose availability. While beneficial in short spurts, prolonged ketosis can lead to the buildup of acidic ketones, resulting in a serious condition known as ketoacidosis. This article explores the intricate processes leading to ketoacidosis, its manifestations, and the importance of timely management.
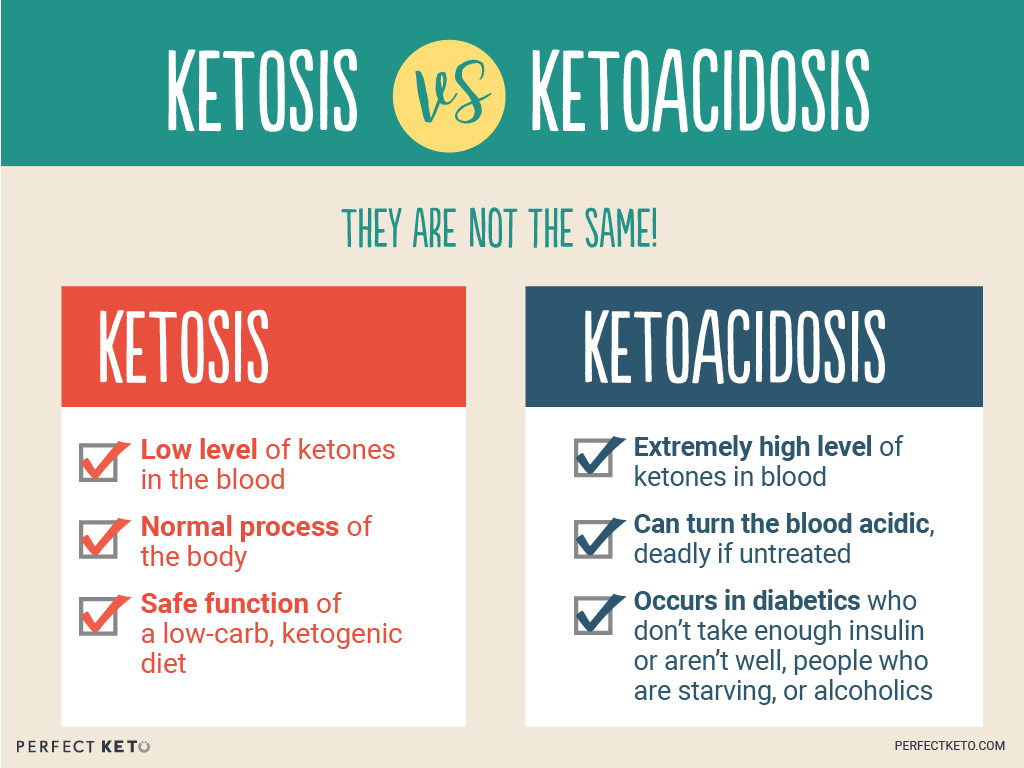
Image: dietdandinobernholtz.pages.dev
Prelude to Acidosis: Unraveling the Ketogenic Pathway
Under normal circumstances, the body derives energy from glucose, primarily obtained from carbohydrates. However, when glucose intake is restricted, as in starvation or certain metabolic disorders, the body switches to alternative energy sources. The liver converts stored fats into fatty acids, which are then broken down into acetyl-CoA. Acetyl-CoA normally enters the citric acid cycle to produce energy.
In the absence of sufficient glucose, acetyl-CoA is diverted to an alternative pathway, producing acetoacetate and β-hydroxybutyrate. These substances, termed ketone bodies, are acidic and accumulate in the bloodstream, a state known as ketosis. While the body can adapt to low levels of ketosis, excessive ketone production can lead to a dangerous buildup of acids.
Manifestations of Ketoacidosis: A Cascade of Physiological Imbalances
A hallmark of ketoacidosis is a profound drop in blood pH, known as metabolic acidosis. As acidic ketones accumulate, the body’s natural mechanisms attempt to buffer the acid buildup, but when overwhelmed, a systemic imbalance ensues.
The body triggers compensatory mechanisms, such as increased breathing to expel carbon dioxide and reduce blood acidity. As a result, individuals with ketoacidosis may experience rapid, deep breathing, known as Kussmaul breathing.
Additional symptoms of ketoacidosis often include nausea, vomiting, dehydration, and electrolyte imbalances. As the condition worsens, confusion and loss of consciousness can occur, posing a life-threatening emergency.
Risk Factors and Underlying Triggers for Ketoacidosis
Individuals with diabetes, particularly type 1 diabetes, are at an elevated risk of developing ketoacidosis. They are more prone to episodes of severe glucose deficiency, triggering the ketogenic pathway.
Moreover, infections, trauma, or medications can increase insulin resistance, worsening glucose metabolism and promoting ketoacidosis. Alcoholism and certain genetic disorders can also contribute to its development.
Image: www.gbu-presnenskij.ru
Management of Ketoacidosis: A Multifaceted Approach
Prompt medical intervention is crucial to reverse ketoacidosis. Management focuses on addressing the underlying cause, rehydrating the patient, and correcting electrolyte imbalances.
Excess ketones are neutralized by administering intravenous fluids containing insulin, electrolytes, and bicarbonate. Insulin helps drive glucose into cells, reducing ketone production. Regular monitoring of blood sugar and ketone levels is essential to gauge the effectiveness of treatment.
Ketoacidosis Results From The Incomplete Breakdown Of
Conclusion: Early Recognition and Intervention are Paramount
Ketoacidosis is a potentially life-threatening condition that requires urgent intervention. Individuals with diabetes should remain vigilant for its warning signs and seek medical attention promptly. By understanding the underlying mechanisms and risk factors associated with ketoacidosis, healthcare professionals can effectively manage and prevent its complications. Early diagnosis and treatment are crucial for reversing the cascade of physiological imbalances and ensuring favorable outcomes.